How Is Precision Medicine Helping the Health Care Industry?
April 27, 2021 - Emily Newton
Revolutionized is reader-supported. When you buy through links on our site, we may earn an affiliate commission. Learn more here.
The traditional approach to addressing an ailment in health care typically involves a physician diagnosing the problem and prescribing a treatment that generally gave the best results to patients who previously had the same complaint.
However, precision medicine takes a wholly different approach by aiming to personalize the intervention to an individual patient. Most people have had frustrating experiences where their doctors prescribe medications that don’t provide the expected relief or even cause unpleasant side effects.
The main advantage of precision — or personalized — medicine is that it targets a patient’s individual characteristics to suggest how to manage their health.
Some broad examples of it in action include:
- Screening people for gene mutations that elevate their risk of developing certain conditions.
- Using genomic sequencing to learn more about how infectious outbreaks make people sick.
- Performing genetic testing on a tumor to determine the best way to treat it.
- Examining someone’s DNA to determine how they respond to particular medications.
Here’s a closer look at how precision medicine benefits the health care sector.
Tailoring Treatment for People Before They Get Sick
It’d be fantastic if someone could look into the future and see which health conditions will eventually affect them. Precision medicine doesn’t go quite that far yet, but it gets close.
Many physicians prefer to practice preventive medicine rather than treating existing disorders. They know it often saves time and money while leading to better life quality for patients.
Suppose a doctor diagnoses someone with prediabetes. They’ll likely give diet, exercise, and lifestyle recommendations to reduce the likelihood of their blood sugar levels getting high enough to fall into the diabetes category. Being proactive like that helps a patient stay healthier and feel more empowered about their well-being.
Precision medicine can go even further. More specifically, some efforts center on preparing the ideal treatments for people before they even show outward signs of illness.
Predicting a Person’s Risk of Heart Failure and Customizing Their Treatments
The American Heart Association recently released a statement about applying precision medicine to people at risk of or experiencing heart failure. It clarified how a person’s gut bacteria, blood biomarkers, and gene variations could predict someone’s likelihood of developing heart failure. This approach may also confirm how a person would probably respond to certain treatments.
The statement also mentioned that typical clinical trials expose large groups to one potential treatment. If it benefits the majority with limited adverse effects, that intervention often gets regulatory approval. However, every clinical trial has participants who have no response to a treatment or experience adverse reactions.
Precision medicine allows health care providers to identify those individuals before such outcomes occur. They can then design new treatments for them that match their unique characteristics. However, precision medicine advocates assert the need to diversify clinical trial participant pools for the most success. They historically feature predominantly white people with specific genetic variants, for example.
Some physicians already rely on precision medicine outside of clinical trial improvements. One option for patients with heart failure is to look at their blood levels of a biomarker called B-type natriuretic peptide. It helps show whether a patient’s condition has worsened or improved. Another benefit is that it can pinpoint whether heart failure causes a person’s symptoms or there’s another ailment to blame.
Applying Big Data to Precision Medicine Advancements
Statistics indicate there’s $165 billion worth of waste in clinical operations every year. However, precision medicine could help minimize it by reducing patient office visits and unsuccessful treatments. Big data is another technology that could achieve gains in this area if health care professionals pair it with precision medicine.
Compiling Data for Enhanced Precision Medicine Outcomes
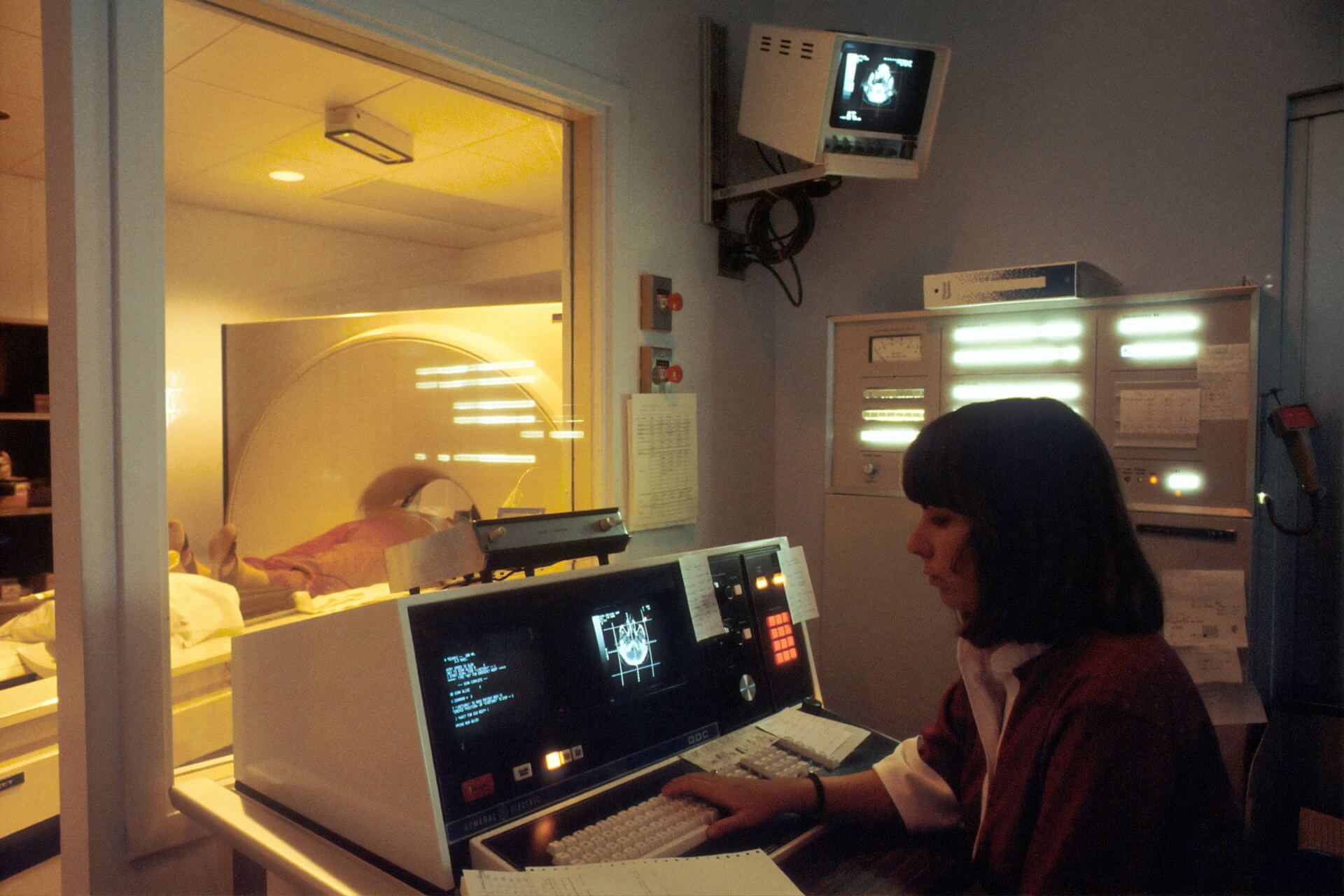
A substantial part of success in precision medicine depends on having accurate data about the individuals getting these treatments. However, a common complication is that information comes from numerous sources. Those could include medical images, physician notes, and health app data.
A European Union project combined big data with artificial intelligence (AI) to create a precision medicine platform that brings information from multiple places into a user-friendly platform. The team then tested their so-called iASiS Knowledge Graph tool by using it for two ailments that medical experts often use precision medicine to treat — dementia and lung cancer.
George Paliouras, who worked on the initiative, explained the approach for someone with Alzheimer’s disease. “By combining data from the patient’s history (e.g. age, sex, smoking, alcohol consumption) with any results of memory tests that may be available, the iASiS platform can assist doctors in deciding on the most likely prognosis of a particular patient.”
Besides aiding physicians in making personalized decisions about patient care, this tool provides suggestions after analyzing different data types. It’s then possible for treatment teams to pursue interventions they may have otherwise overlooked.
Selecting Optimal Treatment Strategies for Patients
Both doctors and patients experience the frustrating reality that some treatments become life-changers for people and don’t have those desirable effects with others. Being diagnosed with the same illness is not enough to guarantee a medical intervention will pay off.
Medical professionals use a combination of their experience, acquired knowledge, research papers, colleagues’ advice, and more to figure out the best ways to help patients. Even then, they’re only human, and the prescribed treatment courses don’t always work.
Precision medicine offers possibilities for analyzing whether a particular intervention will work for a patient before they start it.
Predicting Which Patients Will Respond Best to Exercise
Medical professionals have various possibilities they could recommend for patients. Someone with persistent back pain may ask for a painkiller. However, their doctor might ask them to try posture improvements and a stretching program first. Looking at numerous options is crucial since all medicines have side effects, and some carry the risk of addiction.
A study led by a Rutgers University team assessed how precision medicine could tell which patients with depression would show the best responses to behavioral therapy and exercise.
The investigation involved 66 people with depression. Each participant did either light stretching or moderate aerobic exercise three times per week for two months. The results showed that aerobic exercise reduced depression symptoms by 55% in that group.
The researchers also determined that a person’s reward processing influenced how positively they responded to the exercise regimen. Reward processing concerns how the brain processes rewarding stimuli and modulates a person’s response to positive and negative events.
The exercise did not directly affect reward processing. However, the outcomes confirmed that people with better reward processing at the start of the study were those most likely to see the best results.
Combining Medication and App Usage to Reduce Unwanted Outcomes
Even though many medical practitioners consider precision medicine still in the early stages of its potential, they know that more data opens opportunities to utilize the approach. Fortunately, most people are already familiar with using smartphone apps that can gather data and support precision medicine now and in the future.
Relying on Apps and Medication to Reduce Unwanted Hypertension Treatment Side Effects
Data shows that 45% of United States adults have high blood pressure. Since hypertension increases people’s risk for heart attacks and strokes, physicians usually want to treat it promptly to avoid such complications. They may initially recommend lifestyle changes, then progress to prescribing medication if those don’t work.
The challenging aspect of medication is that it may lower blood pressure while causing bothersome side effects. If those become too severe, some people may decide taking the medicine isn’t worth the associated hassles.
A new precision medicine study aims to find the optimum balance of reduced hypertension with few or no side effects. The research, which will have up to 200 participants, asks people to take prescribed blood pressure medicine while using an app to record their experiences.
The people leading this study also asserted that the approach is an ideal one in the times of COVID-19. The pandemic made many people stay home more often, and that sometimes meant they delayed medical care. Since the app allows participants’ physicians to get real-time data about how the medicine makes them feel, those providers could use it to alter dosages without requiring in-person visits.
Promising Precision Medicine Applications Exist
These examples show that precision medicine could help the health care sector by predicting which populations are most at risk for certain disorders, improving treatment responses and more. Even though some of the case studies here relate to specific conditions, scientists could likely apply the same approach to other health issues.
When that happens, medical professionals will spend less time pursuing treatments unlikely to work for particular patients. They’ll also become more aware of how aspects unique to an individual patient help tell the tale of an intervention’s effectiveness. Thus, everyone benefits.
Revolutionized is reader-supported. When you buy through links on our site, we may earn an affiliate commission. Learn more here.
Author
Emily Newton
Emily Newton is a technology and industrial journalist and the Editor in Chief of Revolutionized. She manages the sites publishing schedule, SEO optimization and content strategy. Emily enjoys writing and researching articles about how technology is changing every industry. When she isn't working, Emily enjoys playing video games or curling up with a good book.