How to Recognize the Symptoms of Hypoxia and Hypoxemia Early
July 29, 2025 - Lou Farrell
Revolutionized is reader-supported. When you buy through links on our site, we may earn an affiliate commission. Learn more here.
Even mild oxygen shortages can snowball from nuisance to medical emergencies in minutes. Hypoxia — too little oxygen in the tissues — and hypoxemia — too little oxygen in the blood — share overlapping signs, but they begin in different physiological neighborhoods. Spotting the earliest cues lets clinicians intervene before organ damage happens. Detection also helps athletes, high-altitude workers or people with chronic lung disease adjust workloads in real time.
Hypoxia vs Hypoxemia
Hypoxemia starts in the bloodstream, lowering the partial pressure of oxygen (PaO2). Hypoxia is the downstream result — starved cells that can’t make enough ATP. One can exist without the other, yet prolonged hypoxemia routinely triggers tissue-level hypoxia. Understanding this cascade is essential when interpreting patient data — correct the blood first and tissue oxygenation often follows.
The Body’s First SOS Signals
Subclinical oxygen deficits are quiet, but they are not silent. In low-oxygen states, the cardiovascular system compensates first, then the nervous system joins the alarm. Recognizing this sequence turns vague complaints into actionable red flags. These early markers often appear before pulse-oximeter values nosedive:
- Subtle neurologic hints: Mild headache, lightheadedness or an “off” feeling that precedes measurable desaturation
- Cardiorespiratory acceleration: Tachycardia and rapid breathing try to move more O2 without changing volume
- Dyspnea on exertion: Tasks that were easy yesterday now leave a person winded
- Cyanosis: Bluish lips, nail beds or earlobes signal hemoglobin less than 85% saturated
- Cognitive drift: Confusion or slowed reaction time, significant for pilots, drivers and machine operators
Tech on the Front Line: Pulse Oximeters and Real-Time Wearables
Pulse oximeters clip onto a finger and estimate arterial oxygen saturation (SpO2) within seconds. They became household names during the COVID-19 pandemic because they warned caretakers when a patient’s silent hypoxemia tipped toward respiratory failure. Coaches for elite cyclists and distance runners also rely on continuous SpO2 feeds to fine-tune altitude training blocks.
Wearable biosensors pair oximetry with heart-rate variability, skin temperature and motion data. Because the devices stream to cloud dashboards, artificial intelligence models can flag deteriorating trends long before a single reading looks bad. Since the devices update in real time, AI will always have up-to-date and accurate information. As a result, it can reference its dataset to make predictions about a user’s health — imagine learning you are at high risk for a heart attack while it is still preventable.
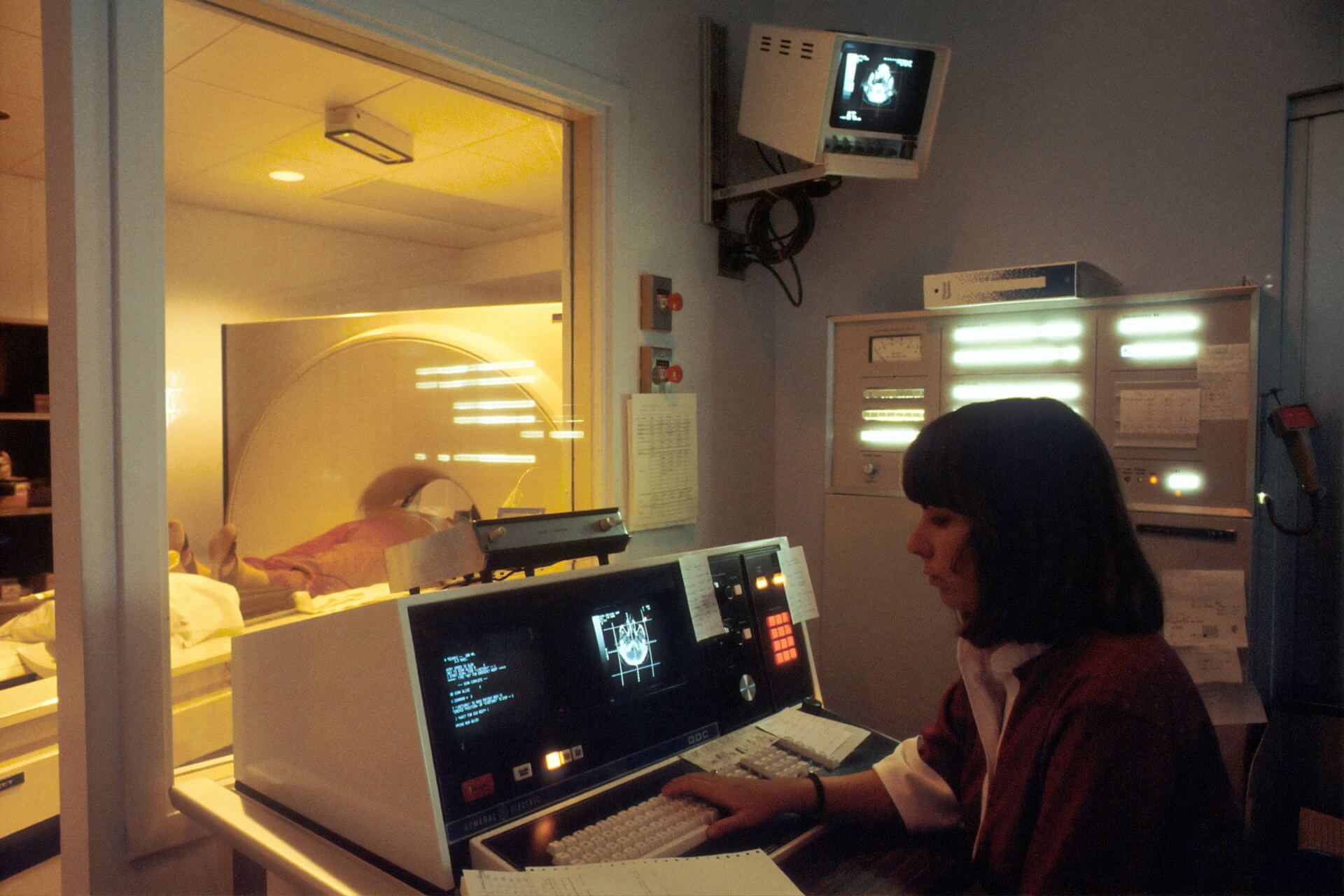
How Medical Professionals Confirm Suspicion
Gadgets raise suspicion — laboratory and imaging tests close the case. Clinicians follow tiered protocols that differ slightly for blood versus tissue deficits but share core measurements.
For suspected hypoxemia, clinicians may order:
- Pulse oximetry: Noninvasive bedside estimate of SpO2
- Arterial Blood Gas (ABG): Direct PaO2 — values under 60 mmHg define hypoxemia
- Six-Minute Walk Test (6MWT): Documents exertional desaturation and functional capacity
For suspected hypoxia, additional tools refine etiology:
- Pulmonary function testing: Distinguishes obstructive from restrictive lung patterns
- Chest imaging: X-rays, CTs or V/Q scans reveal shunts, emboli or parenchymal disease
- Repeat 6MWT with SpO2 telemetry: Highlights discrepancies between rest and exertion
What is a Dangerously Low Oxygen Level? Numbers That Matter
An arterial PaO2 between 75 and 100 mmHg keeps hemoglobin nearly saturated. Dropping below 60 mmHg — or SpO2 under 90% — meets most definitions of “dangerously low oxygen level.” Any reading below these cut-offs demands rapid evaluation and often supplemental O2.
Data-Driven Prediction
When thousands of heart rate, respiratory rate and SpO2 data points flow through machine-learning models, the software can recognize patterns invisible to the naked eye — such as micro-desaturations that precede sepsis or a nocturnal hypoventilation trend hinting at sleep-disordered breathing. Integrating these insights into electronic medical records allows clinicians to move from reactive treatment to proactive prevention.
Best Practices for the Science and Tech Community
Implementing oxygen-monitoring technology involves more than attaching a sensor — it calls for a deliberate strategy that keeps data accurate, interpretable and clinically meaningful. The following best practices help researchers turn raw measurements into reliable and actionable insights:
- Validate consumer devices against clinical-grade oximeters before adopting them for research protocols. Skin tone, nail polish and ambient light can skew results.
- Layer context — combine SpO2 with end-tidal CO2, ECG or barometric pressure data when studying high-altitude physiology or cardiopulmonary rehabilitation.
- Educate users on artifact sources — motion, cold digits — to reduce false alarms.
- Collaborate across disciplines — engineers, clinicians and data scientists should co-design algorithms so outputs address real clinical questions, not just technical curiosities.
Next-generation oximetry chips slot into smartwatches, while optical sensors in earbuds measure cerebral oxygenation. Bio-printed microprobes may eventually monitor tissue oxygenation in transplanted organs. Coupled with federated learning, these innovations promise population-scale insights without sacrificing patient privacy.
FAQs on Hypoxia and Hypoxemia Technology
Can wearable tech detect hypoxia before symptoms?
Yes — trend analysis can spotlight micro-desaturations during sleep or exercise long before a person feels dyspneic.
How accurate are pharmacy-grade oximeters?
Most read within ±2% of ABG-derived saturation in normoxic adults, but accuracy falls in darker skin tones or saturations <80%.
Which populations are hardest to monitor?
Newborns, patients with poor peripheral perfusion and anyone with dyshemoglobinemias — for example, carbon monoxide poisoning.
What is the fastest confirmatory test in the emergency department?
ABG remains the gold standard because it delivers PaO2, PaCO2 and pH in a single cartridge.
Hypoxia vs hypoxemia — why emphasize the difference?
Their treatment targets are not the same. Hypoxemia may need supplemental O2, while hypoxia from ischemia might need clot retrieval or transfusion.
Advancing Oxygen Intelligence: The Road Ahead
Oxygen is medicine, but it is also considered a metric. Marrying traditional pulse oximetry with AI-powered analytics brings critical insight to the wrist, the bedside and the cloud. Whether you are refining an athlete’s VO2 max or safeguarding a COPD patient during wildfire season, the sooner falling oxygen is detected, the faster lifesaving decisions follow.
Revolutionized is reader-supported. When you buy through links on our site, we may earn an affiliate commission. Learn more here.
Author
Lou Farrell
Lou Farrell, Senior Editor, is a science and technology writer at Revolutionized, specializing in technological advancements and the impacts on the environment from new developments in the industry. He loves almost nothing more than writing, and enthusiastically tackles each new challenge in this ever-changing world. If not writing, he enjoys unwinding with some casual gaming, or a good sci-fi or fantasy novel.