5 Main Antibiotic Resistance Mechanisms Explained
November 20, 2023 - Emily Newton
Revolutionized is reader-supported. When you buy through links on our site, we may earn an affiliate commision. Learn more here.
Antibiotic resistance mechanisms are dangerous strategies bacterial strains develop to fight off life-saving medicines. For nearly a century, antibiotics have been saving lives every day and revolutionizing modern medicine. What happens when bacteria evolve to fight off antibiotics, though?
What is Antibiotic Resistance?
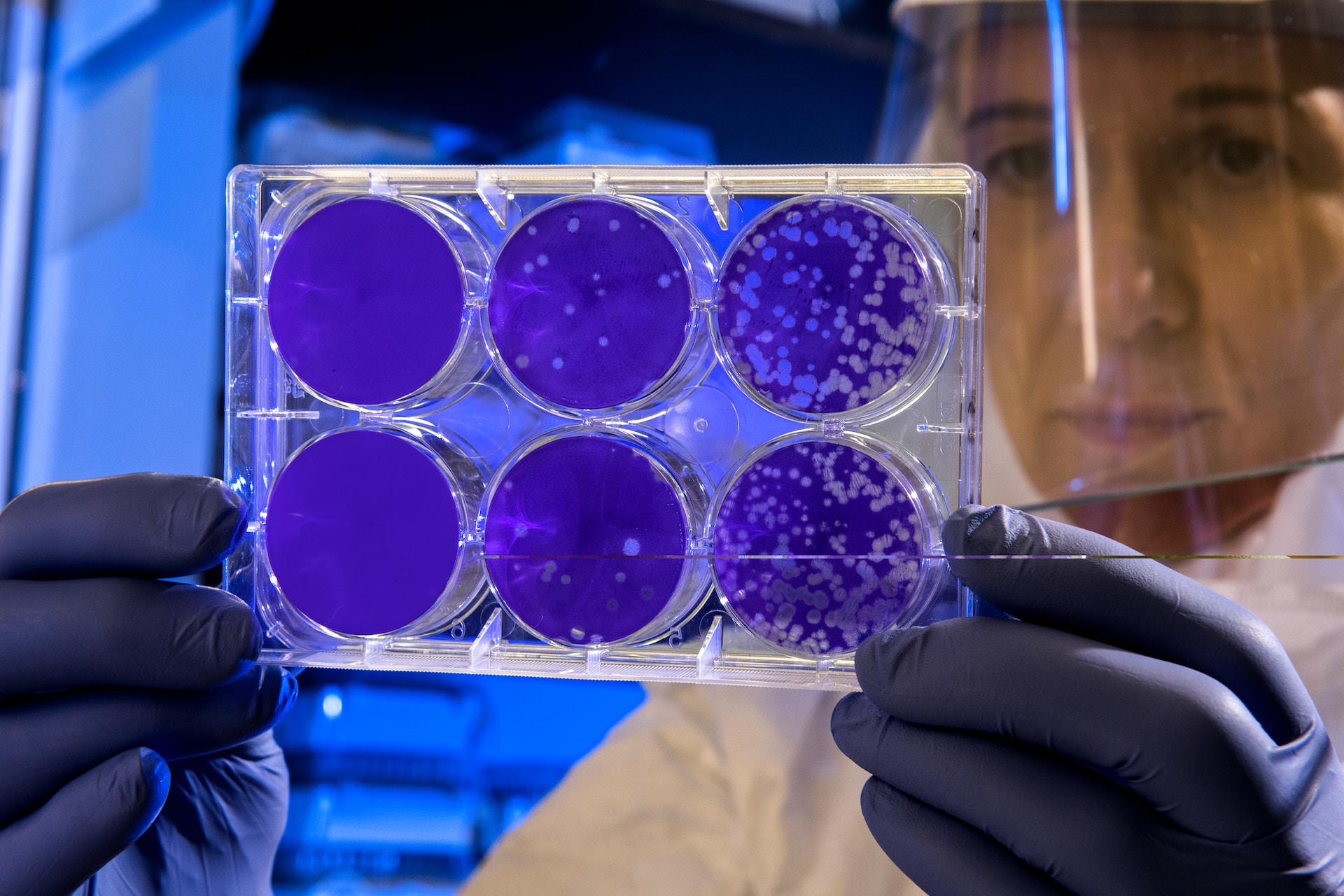
Medicine changed forever when Scottish physician Alexander Fleming discovered penicillin in 1928. Fleming’s discovery was an accident, the result of some mold getting into a petri dish. Penicillin saved millions of lives, though. It was the world’s first antibiotic.
It’s been nearly 100 years since Fleming’s discovery and doctors have developed dozens of other antibiotics since then. Antibiotics fight bacterial infections, preventing and eliminating countless illnesses. Unfortunately, bacteria can evolve to fight back against antibiotics.
This leads to antibiotic resistance, a state where bacteria evolve so much that previously effective antibiotics no longer work. Individual people and animals can’t develop antibiotic resistance – it is a condition in the bacteria, not the patients the bacteria infect. So, there is no vaccine or pill a patient can take to make antibiotics work on them again. Doctors need to develop new antibiotics to counteract the evolved strains of bacteria.
The World Health Organization has identified antibiotic resistance as one of the world’s leading health crises due to its potentially catastrophic impact on healthcare. Doctors are discovering new antibiotics slower than bacteria strains are developing antibiotic resistance. If this trend continues, things could return to a state similar to before the discovery of penicillin since no known antibiotics will work anymore.
The Top 5 Antibiotic Resistance Mechanisms
Antibiotic resistance is a critical concern for doctors and world leaders. It might not be easy to find new antibiotics but, luckily, we do know the main antibiotic resistance mechanisms behind this trend.
An antibiotic resistance mechanism is a trait or behavior that allows bacteria to survive treatments meant to kill them. Doctors are still discovering and studying these mechanisms, but there are five that are particularly prominent.
1. Enzyme Inactivation
Enzyme inactivation occurs when bacteria learn to create an enzyme that nullifies antibiotics. This enzyme is effectively a “magic bullet” that renders the antibiotic harmless to the bacteria. For instance, the enzyme might damage or dissolve the antibiotic so it can’t do its job.
This is easily one of the most common antibiotic resistance mechanisms. It’s essentially basic evolution: the bacteria encounters something that is trying to kill it (an antibiotic drug) and develops a new trait to defend itself (a protective enzyme). This process is like a bacterial version of turtles evolving to have hard shells to protect them from predators.
2. Target Site Modification
The “target site” of an antibiotic is the part of a bacterial cell the drug is designed to identify and attack. If the antibiotic can’t find its target, it can’t deliver the treatment and kill the bacteria. Unfortunately, one of the leading antibiotic resistance mechanisms involves bacteria learning to change the target site and confuse antibiotics.
This antimicrobial resistance mechanism is like a disguise for the bacteria. If the antibiotic can’t recognize the bacteria it’s looking for, it is rendered useless. Bacteria accomplish this in numerous ways, such as altering the number of proteins they have or their cell construction.
Interestingly, target site modification can happen in degrees. Depending on how the bacteria disguises itself, the antibiotic may still be able to bind with it, just not as effectively as it should. So, the antibiotic may still work but the patient will need higher doses of it. Over time, the bacteria will continue to evolve until it is completely resistant to the antibiotic.
3. Efflux Pumping
When humans get sick, we sometimes just “let it run its course”, allowing our body’s immune system to flush out the illness on its own. Bacteria can learn to do this, as well, using a mechanism called an efflux pump. This addition to a bacterium actively pumps out antibiotics as they enter the cell.
Bacteria genetically inherit efflux pumps, increasing the likelihood of antibiotic resistance developing rapidly. As a result, efflux pumps are one of the most concerning causes of antibiotic resistance today. There are several different types of efflux pumps, each of which targets different groups of compounds. Bacteria can develop new efflux pumps or learn to use existing ones to filter out new antibiotics.
4. Restricted Antibiotic Uptake
Some antibiotic resistance mechanisms involve protecting the bacterium by keeping antibiotics outside its cell wall. If the antibiotic can’t get in or isn’t absorbed enough, it will not be able to kill the bacteria. The main method bacteria uses to accomplish this is biofilm formation.
A biofilm is essentially a large protective bubble that surrounds colonies of bacteria. Biofilms are an especially dangerous type of antibiotic resistance mechanism because they also protect the bacteria groups from the entire immune system. Antibiotics may be able to get through biofilms, but it waters down the treatment significantly, leading to higher minimum doses to trigger an effective immune response.
5. Genetic Resistance
DNA is at the heart of evolution, from humans to tiny bacteria. When one organism in a group develops a mutation that allows it to survive longer than other organisms, that genetic trait tends to get passed down. Bacteria can genetically inherit antibiotic resistance mechanisms that make antibiotics progressively less effective on them.
Not all antibiotic resistance mechanisms can get genetically passed down between generations of bacteria. The main types that are eligible for genetic inheritance are drug target modification and antibiotic elimination mechanisms. Interestingly, some genetically-inherited resistance mechanisms can have negative side effects for the bacteria itself, such as slower growth rates.
Resolving Antibiotic Resistance
Antibiotic resistance is one of the most pressing global health challenges today. It jeopardizes decades of research and progress in modern medicine. Doctors and scientists all over the world are working hard to improve their understanding of antibiotic resistance mechanisms and develop ways to address them.
Everyone can take action to help slow the growth of antibiotic resistance, though. Doctors and patients should work together to choose treatment options that don’t include antibiotics if possible. Limiting consumption of antibiotics will help minimize bacteria’s exposure to these life-saving medicines, giving doctors more time to find a solution to antibiotic resistance.
Revolutionized is reader-supported. When you buy through links on our site, we may earn an affiliate commision. Learn more here.
Author
Emily Newton
Emily Newton is a technology and industrial journalist and the Editor in Chief of Revolutionized. She manages the sites publishing schedule, SEO optimization and content strategy. Emily enjoys writing and researching articles about how technology is changing every industry. When she isn't working, Emily enjoys playing video games or curling up with a good book.